Is Uv Light the Same as Blue Light
Product Spotlight – ZEISS Vision Care – UVProtect
UV BEFORE BLUE LIGHT:
Prioritizing Light Protection for the Eyes
By Deborah Kotob, ABOM
Release Date: March 15, 2019
Expiration Date: April 1, 2020
Learning Objectives:
Upon completion of this program, the participant should:
- Learn about UV, its proven biological effects and the known threats to eye health.
- Increase awareness of prevailing misconceptions about still-to-be-determined blue light effects from screen use.
- Learn about the UV protection gap in 4 out of 5 lenses.
- Learn about a clear solution for a known problem: UV radiation damage.
Faculty/Editorial Board:
 Deborah Kotob, ABOM , is currently director of education for Jobson Medical Information LLC, has more than 20 years of experience as an optician. With over 10 years in lens manufacturing as a Sales Consultant, Trainer and LMS content developer. She lectures, trains and conducts webinars on a variety of optical and practice development topics.
Deborah Kotob, ABOM , is currently director of education for Jobson Medical Information LLC, has more than 20 years of experience as an optician. With over 10 years in lens manufacturing as a Sales Consultant, Trainer and LMS content developer. She lectures, trains and conducts webinars on a variety of optical and practice development topics.
Credit Statement:
This course is approved for one (1) hour of CE credit by the American Board of Opticianry (ABO). Technical Level 2 Course STJHI007-2
Support:
This course is supported by an educational grant from ZEISS VISION CARE.
We have a duty as eyecare professionals to educate the patient about controllable threats to their eye health. We do a disservice when we don't educate them on ways to reduce risk factors for UV damage to their eyes. By proactively limiting their lifetime UV light exposure from childhood, patients can reduce UV-induced damage to their eyes. A lifetime of cumulative irreversible photo damage can become a threat to their eye health and even their sight. Moreover, equally important, we have a duty to offer eyewear lens solutions with the highest level of protection from these irrefutable threats.
MISCONCEPTIONS ABOUND REGARDING UV AND BLUE LIGHT PROTECTION AND PRODUCTS
Counter to what many ECPs believe, UV is not a problem that has already been solved! Many ECPs have firm but misguided beliefs about the level of UV protection that existing lenses provide. We mistakenly believe that clear lenses like polycarbonate already have full UV400 protection built in.
Why are we talking about prioritizing light protection for the eyes? In eyecare, the conversation surrounding light protection for the eyes has become hyper-focused. Alarmingly, the focus is not on the proven high-level threat to the eye from the harmful effects of UV radiation (UVR) exposure. Instead, our focus increasingly centers on the purported blue light hazards from digital device screen emissions. The harmful eye health effects of UV radiation exposure are obscured by the media buzz surrounding blue light risk from digital devices, whose long-term harmful effects remain highly inconclusive.
Compounding the confusion around light protection is the fact that industry veterans and new ECPs alike have been caught up in the momentum around blue light, where scientific findings are still in flux. For example, ECPs are often under the mistaken belief that a blue filter AR or a lens filter blocks a high percentage of blue light when in fact the reduction and therefore the protection is quite minimal. It is difficult for the ECP to sort through the inconsistent and often conflicting information and claims to make informed decisions. For example, which wavebands of blue light are considered harmful long term versus those that may contribute to digital eye fatigue?
Dispelling firmly held misconceptions is challenging, but this course will give the facts and supporting science-based data from which we can reframe our understanding of UV protection in lenses, the blue light hazard from screen use and the undisputed dangers posed by UV radiation exposure to the eyes, particularly young ones.
In this course, you'll be given information to help you understand the need to extend UV protection to UV 400 nm in lenses, beyond the current 380 nm ANSI/ISO standard for "100 percent UV protection." This course addresses the vital need to refocus the light protection conversation on the dangers posed by UV radiation to the eye and surrounding skin tissues. We will provide a perspective on the blue light hazard, and the lenses and coatings purported to attenuate them. Finally, you will learn about a product that provides increased UV protection in a clear lens.
WHAT IS UVR?
UVR is light energy that ranges from 100 to 400 nm on the electromagnetic (EM) spectrum.
Ultraviolet rays are invisible. The word means beyond violet (beyond visible violet light): Violet is the highest energy visible light that borders UVA on the electromagnetic spectrum. Shorter wavelengths produce EM waves of a higher frequency and therefore higher energy. So blue visible light has a longer wavelength and therefore contains less energy than UVA. UVA contains less energy than UVB. UVR is actinic light meaning that it has energy levels high enough to produce photochemical damage to biological structures when absorbed. The ability of actinic UV light to harm the eyes or skin is wavelength dependent. Different layers of skin and eyes absorb specific ranges or bands of wavelengths. Higher energy waves are primarily absorbed by the outer layers of the skin and eyes, while longer, less energetic waves penetrate deeper into tissues of the skin and eyes. Only two parts of our bodies absorb and are susceptible to damage by light, the skin and the eyes.
"The primate/human eye has unique filtering characteristics that determine in which area of the eye each wavelength of light will be absorbed. Both UV-A and UV-B induce cataract formation. The removal of these wavelengths from ocular exposure will greatly reduce the risk of early cataract formation," states Joan E. Roberts, PhD, in "Photobiology of the Lens." (photobiology. info/Roberts.html)
UVR EFFECTS ON EYE HEALTH
UVR is an undisputed threat to eye health. Scientific and international regulatory bodies agree: UV is harmful to the human eye and its surrounding tissues. UVR is EM radiation that can cause ocular oxidative photodegradation that can result in severe damage to the eyes and their surrounding structures. While UV contributes little to nothing to sight, it can severely damage the eyes and their surrounding structures.
UV interacts strongly with molecules in human cells. Research has shown that the effects of UV damage accumulate over a lifetime; early and frequent retinal exposure may contribute to age-related macular degeneration later on in life. Other known effects of UV exposure include:
- Photo-aging of the eyelids and surrounding skin.
- Skin cancers of the same regions, accounting for up to 10 percent of all skin cancers.
- Degenerative and unsightly growths on the conjunctiva.
- Acute and painful inflammation of the cornea.
- Melanoma of the iris, a potentially deadly type of cancer.
- Nuclear sclerosis of the lens leading to reduced vision and ultimately to cataracts that require surgery.
DAMAGE AND DISEASE
CAUSED BY UVR
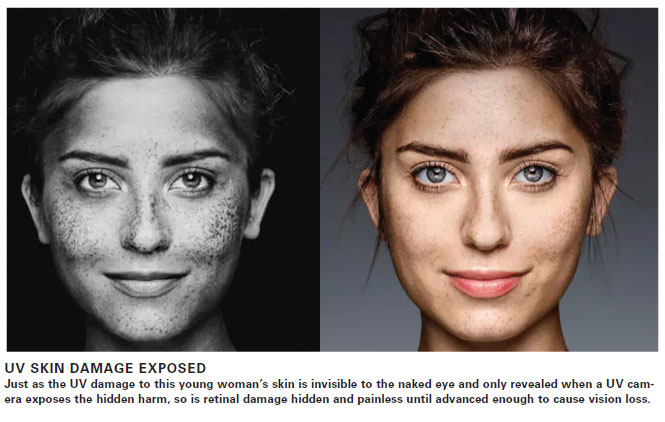
The damage caused by UVR can be acute or chronic. Acute damage occurs with short but intense exposure. Most acute damage is painful and temporary, and will heal. Chronic damage and subsequent disease development are caused by much lower levels of exposure over a long period, often many years. Chronic damage is phototoxic and photo-aging. It accumulates over a lifetime, and there is no cure—the damage is irreversible. Chronic conditions are insidious, and because they happen gradually, they go undetected until significant irreparable damage is present.
Conditions caused by UVR include:
Eyelids and periorbital skin: UVR damage to the eyelids is common. Sunscreen should be applied to the eyelids to prevent injury, but research indicates that people are noncompliant because of eye irritation.
Skin: UVR exposure results in photo-aging of the eyelids and surrounding skin. UV photo damage thickens the skin resulting in deep premature wrinkles. UVR damage to sebaceous glands can lead to xerosis (dry skin). Actinic keratosis is an advanced type of damage to the skin characterized by dry red patches; it is considered pre-cancerous. Eyelid cancers represent 5 to 10 percent of all skin cancers and can easily metastasize or spread.
Cornea: Ultraviolet keratitis, also known as photokeratitis, is a painful eye condition caused by exposure to ultraviolet rays. It can be referred to as sunburn of the cornea.
Conjunctiva: A pinguecula is a thickened deposit of fat, protein and calcium that is visible over the white of the eye. Unless it grows into a pterygium, it usually is only an unsightly cosmetic problem.
Iris: Melanoma tumors are the most common cancer of the eye, and evidence suggests that UVR is one of its leading causes. When located on the iris, the most common location is at the bottom, where daylight UVR exposure is strongest.
Lens: UVR causes pre-cataractous changes by causing proteins to clump together. As the eye ages, protective pigments in the lens convert to pigments that react to UVR, further damaging the outer layer of the lens and lens proteins. When enough damage has accumulated, cataracts develop. Both UV-A and UV-B induce cataract formation. In "Biology of the Human Lens," Joan E. Roberts states: "The removal of these wavelengths from ocular exposure will greatly reduce the risk of early cataract formation. If you prevent light from exciting endogenous or exogenous chromophores in the lens, or you block the damage of reactive oxygen species with antioxidants, you may prevent or retard cataracts from forming." (Roberts 2008, photobiology.info/Roberts.html)
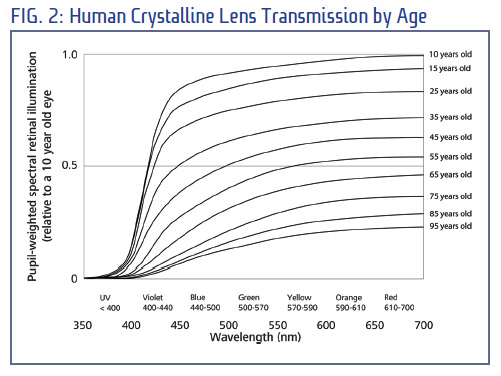
Retina: In young eyes, a significantly higher amount of UVR reaches the retina due to the fact that their crystalline lens has not yet developed the proteins that absorb UVR and shield the retina from this high energy light exposure. Consequently, they are at a higher risk of photochemical damage occurring in their retinal cells. The retina is susceptible to photochemical damage which occurs because of chemical (oxidative) reactions induced by absorption of high energy photons. The highest energy photons that reach the retina are from ultraviolet radiation. UV transmission reduces with age, but those in their teens, 20s and 30s still have significant amounts of UV reaching their retinas.
DIGITAL DEVICE SCREEN EMISSIONS AND BLUE LIGHT!
Blue light product claims often imply a high level of protection for the retina. And claims of retinal damage from screen use are unsubstantiated. Despite conflicting studies regarding the blue light emission levels from digital devices and their ability to produce harmful effects, and despite the fact that very limited protection is provided by clear blue filter lens products, the blue light topic has unfortunately eclipsed the irrefutable UV threats to eye health. Simply put, the health risks from UV are real, well documented and therefore, our communication with the patient regarding light protection must convey the higher level and immediate threat posed by UV radiation exposure.
BRINGING CLARITY TO THE BLUE LIGHT BUZZ
The case for the blue light hazard harming eyes exposed to digital device screens is tenuous at best.
Recently, there has been growing concern about visible blue wavelengths between 400 and 500 nm—the spectral region associated with blue light hazard (BLH). Some studies have linked long-term exposure to blue light in sunlight to macular degeneration. Other research has contradicted these claims while many blue light studies have notable shortcomings.
For these and other reasons, the U.S. National Eye Institute has no formal position regarding blue light.
BLUE LIGHT HYPE IN THE MEDIA?
Unfortunately, the media has misunderstood blue light's potential eye damage risks. The University of Toledo showed in a study that blue light could damage the retina. However, the study exposed human cells in vitro to 445 nm using a blue laser concentrated at only one wavelength, to examine the damage induced. While this makes for sensationalist headlines, this is clearly not representative of real-world conditions.
Many press outlets interpreted the study to mean blue light from electronic devices can severely injure retinas. For example, a headline from Fortune Magazine stated: "Blue Light Emitted from Electronics Can Cause Accelerated Blindness, Study Finds."
If blue light has the potential to harm our retina, then natural outdoor light presents a far larger risk than any digital source. Outdoor blue light produces many orders of magnitude higher dose of blue light with natural sunlight being many times brighter than any digital display (even when these are on the brightest settings).
There is a serious disconnect between the findings in the study and media stories. Given the current state of scientific evidence, the long-term eye health risk of blue light from digital devices is premature and likely overstated.
The debate and controversy over blue light will likely remain for a while, but we can confidently recommend UV protection based on proven well-established peer-reviewed scientific and clinical data. Eye health and light protection conversations can certainly include blue light, but first and foremost, we have a duty to warn and protect patients of the danger that UV poses to their eyes.
THE PROBLEM WITH CURRENT OPHTHALMIC LENS UV STANDARDS
Exposure to UVR hazards can occur from artificial light sources such as welding arcs, tanning lamps, UV sterilizers and UV curing lamps. Although these sources can cause immediate damage, the acute effects are usually short-lived and reversible. However, it is exposure to natural UVR outdoors that presents the greatest threat. Highly respected medical and scientific organizations like the World Health Organization and the American Cancer Society, all define the UVR spectrum as extending to 400 nm. Ophthalmic lens, industry standards organizations, however, are inconsistent in their definition of the UVR spectrum range.
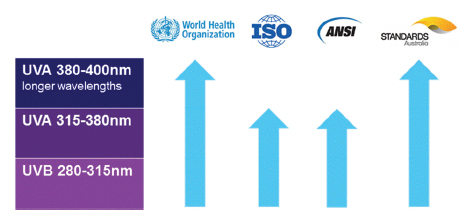
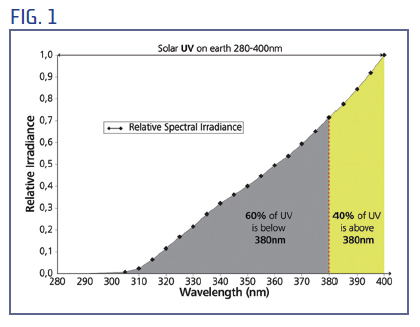
For example, the ISO ophthalmic lens standard (ISO 13666:2012 – Ophthalmic optics - Spectacle lenses Vocabulary) refers to an average solar daylight spectrum but defines the upper limit of UV radiation to be at 380 nm. By this definition, 40 percent of solar UVR exposure on Earth's surface is within a spectral band that is ignored by this standard. In contrast, the Australia/New Zealand sunglass standard (AS/NZS 1067:2003. Australian/New Zealand Standard. Sunglasses and fashion spectacles) defines UVR as ending at 400 nm.
UV EXPOSURE AND THE EYE
The way that UVR reaches the eye and its surrounding structures depend on several climatic and geometric factors. Intense exposure may happen even on hazy or partially cloudy days. The greatest UVR exposures often occur in mid-morning and mid-afternoon, not at noon as many are inclined to believe. Around noontime, the eye itself is typically not exposed to the direct rays of the sun. Much more ocular UVR exposure can come from reflection from surfaces below the eye and by atmospheric scattering. UV levels increase with altitude, therefore, those living or playing in the mountains experience higher levels of UV exposure as do those living at or near the equator where the sun is closest to the earth.
Exposure rates vary with age as illustrated in Fig. 2. A portion of the UVR spectrum reaches the retina in a young person's eyes that is largely absorbed by anterior structures of the adult eye. The very young have the highest level of UV transmittance to their retinas and therefore the highest exposure. Gradually, the transmittance of UV to the retina diminishes but remember that any UV reaching the retina is damaging, and the damage is cumulative and irreversible. Certain medications and supplements increase the intensity of UVR, its damaging effects and the rate of damage. The mechanism for increasing damage is due to their photosensitizing effects.
"Photosensitizers are molecules that can be activated by light in order to generate reactive oxygen species (ROS) that can damage cell structures from microorganisms or from diseased mammalian cells leading to cell death." (From Nanobiomaterials in Antimicrobial Therapy, 2016).
For those who sunbathed while taking an antibiotic and suffered a severe sunburn, you have experienced the effects of photochemical damage from photosensitizers. Something as simple as aspirin is a photosensitizer, and many blood pressure drugs are as well. Both the skin and eyes are at a higher risk of harm from UVR when photosensitizers are applied to the skin or ingested. Knowing that circumstances abound which place our eyes and our customer's eyes at higher risk of UV damage, it is incumbent upon us to ensure that every patient is armed with this information. We all deserve the opportunity to be pre-emptive in protecting our health including our eye health.
Also, keep in mind that UV transmittance to the retina increases dramatically in those who have had a cataract removed and replaced with a clear intraocular implant (IOL). Although newer IOLs have some UV protection built in, they do not protect up to UV400 nm. Also, this new influx of UV is impinging an aged eye that has already accumulated a lifetime of damage making their retinas even more susceptible to damage. Those with light colored eyes, blue or green, are more susceptible to the harmful effects from UVA because of higher transmission levels that pose a threat for increased cancer risk.
UVR EXPOSURE FOR THE EYEGLASS WEARER
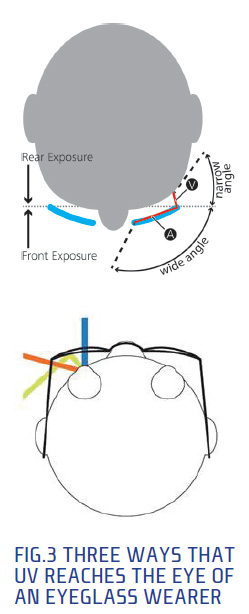
Four out of 5 eyeglass lenses do not block 100 percent of UV up to 400 nm from passing through the lens, including most polycarbonate lenses. However, new technology exists (e.g., ZEISS UVProtect) that does. And with this level of UVR attenuation, eyeglasses can provide significant protection from UVR exposure for the eyeglass wearer. Considering that the vast majority of UVR enters the lens from the front, it's vital to have a lens that prevents it from passing through to the eye.
In a recent peer-reviewed study, UVR irradiance was measured using a specially designed mannequin to simulate real-world conditions. In this study, 94 percent or more of UV strikes the front of the eyeglasses while a maximum of 6 percent reached the eye from other angles not blocked by the eyeglasses. And it was greatest when the mannequin faced toward the sun, likely due to the greater intensity of direct sunlight reflecting off of spectacle frames and facial features of the mannequin. Some of the rearward UVR will miss the face and pass into the lens. Although you will hear that these rays will reflect into the eye only, a perfect UVR mirror could return all of those rays to the face. The total UVR irradiation traveling through the front of the lens is up to 20 times larger than the UVR irradiation passing from behind the wearer.
This is in stark contrast with the claims of one industry paper which states that a significant portion of hazardous UVR exposure to the eye (approximately 50 percent) is reflected from the back surface of spectacle lenses. This data in this paper is not only old and flawed, but it has, regrettably, helped foster a false sense of security in our industry that back coating UV ARs can significantly reduce UV exposure.
The repercussions of UVR exposure should be clear for the eyecare professional and the eyeglass wearer: For many wearers, the greatest potential exposure may occur when wearing clear lenses outdoors. Most of the UVR that can reach the eye and eyelids strikes the front of the spectacle lens first. It is therefore imperative for clear spectacle lenses to render it harmless; all of it, up to 400 nm.
CLEAR PROTECTION
 The best way to protect our eyes is to provide sunglass-level protection in a lens that blocks UV fully up to 400 nm and to start protection at an early age.
The best way to protect our eyes is to provide sunglass-level protection in a lens that blocks UV fully up to 400 nm and to start protection at an early age.
For example, clear lenses with UV protection up to 400 nm without any noticeable tint (e.g., ZEISS UVProtect lenses), are effective because they filter UV in the substrate and therefore prevent its transmission through the lens and to the eye.
The risks of UV exposure over a lifetime is well documented, making it imperative that we provide patients with eyeglass lenses that include full UV400 protection. We must not ask our patients to settle for less protection simply because the ANSI and ISO standards permit claims of "100 percent UV protection" for lenses that only protect up to 380 nm while still allowing 40 percent of UV radiation to reach our eyes.
ZEISS, in particular, has closed this significant UV protection gap by including UVProtect technology in all ZEISS clear plastic lenses. This technology provides the highest level of UV protection in a lens. UVProtect technology blocks UV wavelengths up to UV400, and ZEISS UV Protect lenses maintain clarity with no noticeable tint, which is a challenge in lenses that block up to UV400 and provide sunglass level protection in a clear lens.
In conclusion, the most popular clear spectacle lens materials do not completely block the most plentiful source of UVR, the solar spectrum between 350 and 400 nm. Some ophthalmic lens standards ignore the hazard of UVR wavelengths longer than 380 nm and up to 400 nm, creating a UVR protection gap.
Eyeglass wearers typically are aware of some of the damaging effects of UVR, but many incorrectly think that their eyeglass materials or coatings already provide complete UVR protection. In many cases, their eyecare professionals have been led to the same inaccurate conclusion.
Ophthalmic prescription lens standards for UVR are derived from studies of damage caused by short high-intensity exposure to UVR to structures only in the eye itself. The eyelids are perhaps even more susceptible to UVR damage. The cumulative damage to the skin from low-level exposure to UVR over many years is well documented, but many people will not apply sunscreen on their eyelids.
Recent research suggests that the action spectrum used in some ophthalmic lens standards does not solely represent the risk to the eye itself and that further spectra should also be considered. It is worth noting that cosmetic and sunscreen industries all use the 400 nm UV standard in the development of their skincare products.
As we understand more about photo-aging and pre-cataract changes to the lens of the eye, it is becoming apparent that longwavelength UVR is more important than previously thought.
This damage may be amplified by medications or herbal supplements that increase photosensitivity that in turn increase the amount of damage incurred.
All of this makes it imperative that lenses provide the highest level of UVR protection or UV400.
The light protection conversation must return to increasing awareness amongst patients of the eye health threat posed by UVR. The blue light conversation certainly deserves to happen, but it must be put in its proper place and delivered from a more pragmatic perspective.
Source: https://www.2020mag.com/ce/uv-before-blue---prioritizing-lig
0 Response to "Is Uv Light the Same as Blue Light"
Post a Comment